In order to keep up the fight against COVID-19 and other dangerous pathogens, it is important that countries have access to reliable and accurate information about the disease. The best way to do this is by training healthcare workers in all areas of COVID-19 detection and testing, as well as tracing and tracking methods.
Healthcare workers must also be able to ship samples safely between facilities so they can be tested at different levels of care.
Defending for COVID-19: racing against time
Diagnosing COVID-19 is challenging. It’s likely that many of the people who have contracted it won’t show symptoms for weeks or even months, meaning they could be walking around without knowing they’re carriers. And since there are no vaccines or treatments available yet, a timely diagnosis is vital to saving lives: earlier detection means better chances of survival.
Tracking: linking community with health system

You’re probably wondering what a tracing and tracking system is. It’s a way of helping countries keep up the fight against COVID-19 by linking communities with health systems. A strong health system is needed for this because it can:
- Reach those who need care
- Provide support to community members who have been affected by the disease
- Help stop further cases from spreading in the future
Shipping and transporting of samples

The first step in fighting COVID-19 is to prevent it from spreading. To do so, samples must be taken from infected patients and sent to labs for testing. This can take place at the point of origin or at a border crossing. Given the nature of the disease, however, some communities are more remote than others and therefore harder to reach.
The challenges of transporting samples over long distances include maintaining cold chain (keeping them at temperatures below 4 degrees Celsius) as well as ensuring that samples do not mix with other cargo or with people during transport (which would compromise their purity). Additionally, coordination between all stakeholders involved in this process is required to ensure that proper procedures are followed and there are no delays in shipment delivery times due to customs inspections or other bureaucratic hurdles.
Treating for COVID-19: equipping treatment centres with oxygen

Oxygen is the most important tool in the fight against COVID-19. The gas helps patients breathe, but it can also be used to treat the disease itself. This treatment is called hyperbaric oxygen therapy (HBOT).
The main purpose of HBOT is to increase the amount of oxygen available in your blood and tissues by using higher than normal pressures and concentrations of oxygen, which causes more molecules to enter your bloodstream. Because COVID-19 attacks cells that are deprived of oxygen, more oxygen means a stronger immune system and better chance at recovery.
In order to do this successfully, there are several factors that need to be taken into account:
Maintaining essential health services: protecting the precious health gains

The World Health Organization estimates that maintaining essential health services is crucial to keep up the fight against COVID-19. As the virus spreads, WHO has called for countries to invest in their health care systems and ensure they can provide basic services to people at risk of contracting the disease.
Health care is a human right, enshrined in international law by treaties such as the Universal Declaration of Human Rights and more recently with specific articles within the Paris Agreement on Climate Change. The Sustainable Development Goals also include targets for universal health coverage (UHC), which means everyone has access to quality medical care without discrimination based on age or economic status.
We’re all in this together.
The fight against COVID-19 is a global effort. We must work together to protect our health, to protect our children, to protect our communities and families. It’s not just about one country or one region; there is no time for borders when it comes to the safety of your loved ones.
COVID-19 can be deadly in any country if proper precautions aren’t taken. As such, we must all take part in this fight by protecting ourselves and others from exposure and infection with common-sense methods like hand washing and staying home if you feel sick with flu-like symptoms.
The agency’s work is focused in the following areas:

To help countries prepare for, detect and manage outbreaks:
- Understand the virus and its transmission patterns
- Build capacity to respond quickly to new cases in health facilities through training and supplies.
- Provide guidance on how to treat patients with basic care needs, such as rehydration or oxygen support.
To protect health workers and others who may be exposed during an outbreak:
- Ensure that people who are at risk of getting infected have access to antiviral drugs (when recommended), vaccines (when available) and personal protective equipment like gloves, masks, etc., so they can reduce the risk of contracting COVID-19 themselves or spreading it to others.
The WHO also works on communication with the public about how they can stay safe from this deadly disease including through social media channels such as Facebook Live which is being used by some countries including Japan where there has been a large number of confirmed cases since October last year.
Preparedness for health emergencies

The WHO Emergency Preparedness Framework is the starting point for countries to develop and implement their national emergency preparedness plans. The Framework was developed by WHO in collaboration with the Inter-Agency Standing Committee (IASC) and other partners, including the Food and Agriculture Organization of the United Nations (FAO), Centers for Disease Control and Prevention (CDC), United Nations Children’s Fund (UNICEF), World Bank, International Federation of Red Cross and Red Crescent Societies (IFRC), Médecins Sans Frontières/Doctors Without Borders (MSF) and others.
The Global Health Emergency Management System is a network that enables real-time information exchange between governments, agencies, non-governmental organizations (NGOs), international organizations and individuals involved in global health emergencies response efforts around the world.
This system provides guidance on how to prepare before an event occurs; train staff appropriately; respond quickly during an emergency; coordinate with all partners during an event; assess needs after an event occurs; provide humanitarian assistance where needed; maintain public awareness about ongoing emergencies on a regular basis through social media platforms such as Twitter or Facebook; recover from any damage caused by an emergency situation when possible so that normal operations resume as soon as it makes sense logistically speaking
Detection and reporting of outbreaks

WHO is working with partners to improve detection and reporting of outbreaks in the WHO Africa region. This includes countries working together, sharing information, and using a common approach to detecting outbreaks.
In addition, the WHO African Region has established a network of laboratories that can test for COVID-19. The network provides results within 48 hours, which allows for quick action to contain outbreaks once they are detected.
Laboratory testing and surveillance for COVID-19
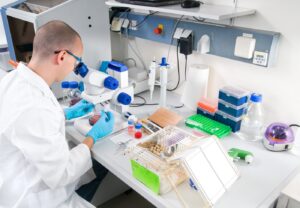
- Testing for the virus is important, because early detection can help to stop the spread of COVID-19.
- If you think you have COVID-19 and are experiencing flu-like symptoms, please see a health care provider immediately.
- You may want to contact your local health department or visit the Centers for Disease Control and Prevention website to find out more about where to get tested for COVID-19. If you do test positive, your doctor will give you treatment and advice on how to avoid infecting others until it’s safe for them to return home.
Protecting health workers from infection and providing psychological support

- Protecting health workers from infection
- Providing psychological support
The importance of protecting health workers from infection cannot be overstated. The best way to protect yourself is to avoid contact with infected body fluids, such as blood and saliva. If you have been in contact with someone who has measles and has not been vaccinated against measles or had a previous case of the disease, you should be vaccinated within three days.
It’s also important that you wash your hands often, cover coughs and sneezes using tissues or face masks, avoid touching your eyes after coming into contact with an infected person’s bodily fluids (including mucus from the nose), stay home if you are feeling unwell and use antiseptic solutions on surfaces in public areas like buses or trains where others may sit upon them later on – especially if they’re used by children.
Risk communication and community engagement
Risk communication is the process of exchanging information between a health authority and a community to reduce the risk of disease transmission. It’s an essential part of any response to a public health emergency, and it’s part of several WHO pandemic preparedness frameworks. Communities play an important role in preventing outbreaks by practicing good hygiene and reporting suspicious symptoms at their nearest health facility. They also serve as sentinels for emerging diseases, since they’re often quicker at spotting changes in behaviour than official networks are.
In this section we’ll look at some examples from across the world that illustrate how communities have helped keep up the fight against COVID-19 over the past year – from changing behaviours around travel restrictions during the outbreak in Hong Kong to communicating with people affected by dengue fever on social media platforms like WhatsApp in India.
Emergency medical response are in over 100 countries around the world.

Gender equality is an essential part of every aspect of life, whether it’s health or emergency response.
The world has seen many examples where women have had to take on the role of supporting their families after their husbands or partners have died from COVID-19. In fact, in some countries like Lesotho and Liberia, women are being told not to send their daughters to school because they cannot afford both food and school fees for them.
These gender inequalities mean that people affected by COVID-19 will continue to suffer without access to proper medical care or advice about how best to protect themselves against catching this virus.
This is why we need gender equality at the heart of all policy responses so that we can build strong communities that support survivors and ensure everyone has equal access to vital services like education, healthcare and cash transfers when needed most
Need the best guidance and assistance that we can give them.

As we work together to prevent and control this pandemic, we need to remember that countries and communities hit hard by COVID-19 need more than just funding. They also need our best guidance and assistance in order to manage their outbreak.
WHO is working with partners around the world to provide technical support for countries responding to COVID-19. The WHO response plan outlines roles and responsibilities for national governments, WHO staff members, other UN agencies and other health partners.




